I am currently involved in two clinics at UT Health in Austin evaluating people for small fiber neuropathy (SFN). The first clinic was one I initiated with the Neuroimmunology group to look at patients with a diagnosis of Fibromyalgia, since studies currently demonstrate that approximately 40% of these patients test positive for small fiber neuropathy. Within that clinic I have also began evaluating people with a diagnosis of MS. The second clinic is with the Post-acute sequalae of COVID clinic (PASC for short), we find many people with symptoms consistent with SFN in this group.
I compiled the below information for my patients to help them better understand their new diagnosis as it is something that has been poorly understood up until the past few years.
Overview
Small fiber neuropathy (SFN) occurs when the small fibers of the peripheral nervous system are damaged. Small fibers in the skin relay sensory information about pain and temperature. In the organs, these small fibers regulate automatic functions such as heart rate, sweating, digestion and sexual function.
A diagnosis of SFN can be a sign of an underlying health condition. Often, though, no underlying cause is identified.,
Small fiber neuropathy is a type of peripheral neuropathy, meaning that it does not affect the brain or spinal cord. With small fiber neuropathy, the smallest nerve fibers of the peripheral nervous system are affected. These fibers have little to no protective myelin on them and they communicate directly with the immune system which makes them vulnerable to damage from inflammation or infection in the body.
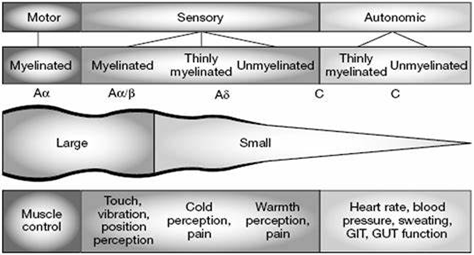
The small thinly myelinated/unmyelinated A and C fibers are involved in the perception of pain and temperature as well as the autonomic control of organs as illustrated below:
Symptoms
Symptoms of small fiber neuropathy can vary. Sensory symptoms that may be seen are:
- Burning, tingling, itching or prickling
- Short bursts of pain
- Sensations of vibration in the body
- Loss or dulling of sensation
Some sensory symptoms can be caused by external triggers. For instance, some people might experience foot pain when wearing socks or touching bedsheets.
Symptoms can be mild or severe, though early symptoms are often mild. Small fiber neuropathy may affect the feet first and progress upward. It can affect all other parts of the body as well and may not follow any particular dermatomal pattern.
In some cases, small fiber neuropathy disrupts autonomic functions. Autonomic functions are things your body does automatically, such as regulating digestion, blood pressure, and urinary function.
When autonomic nerve fibers are affected, symptoms can include:
- Constipation
- Sweating (decreased or increased)
- Dizziness
- Dry eyes
- Dry mouth
- Incontinence
- Sexual dysfunction
- Skin discoloration
- Exercise intolerance
- Tachycardia/Bradycardia
- Orthostatic intolerance
- Nausea, reflux
Causes
Small fiber neuropathy can be the first sign of an underlying condition, such as diabetes. Other conditions that may cause small fiber neuropathy include:
- Endocrine and metabolic disorders
- Hypothyroidism
- Metabolic syndrome
- Hereditary diseases
- Fabry disease
- Hereditary amyloidosis
- Hereditary sensory autonomic neuropathy
- Tangier disease
- Immune system disorders
- Celiac disease/Gluten Intolerance
- Inflammatory bowel disease
- Lupus
- Mixed connective tissue disease
- Psoriasis
- Rheumatoid arthritis
- Sarcoidosis
- Scleroderma
- Sjogren’s syndrome
- Vasculitis
- Infectious diseases, such as viral infections
- Hepatitis C
- HIV
- Lyme disease
- Certain medications, such as chemotherapy drugs
- Vitamin B-12 deficiencies
- Alcoholism
When you are diagnosed with small fiber neuropathy, we evaluate you for all of the above mentioned conditions, though in as many as 40% of cases no cause can be found. In the instances in which no cause is found, the small fiber neuropathy is considered idiopathic.
Risk factors
Not everyone with the above conditions will get SFN, but having one or more of the conditions listed may put you at an increased risk of developing small fiber neuropathy.
Diabetes is the most common risk factor for this condition. Research suggests that around 50% of people with diabetes will develop a diabetic neuropathy in their lifetime. Though small fiber neuropathy is less common than other types of diabetic neuropathies, it’s important to take into consideration.
Studies have also shown that people with idiopathic small fiber neuropathy have a higher prevalence of impaired glucose tolerance than the general population. Impaired glucose tolerance is associated with prediabetes. Small fiber neuropathy may be one of the earliest signs of prediabetes.
Age is another risk factor. Small fiber neuropathy is most commonly seen in people over the age of 65 than in younger individuals. Poor nutrition and chronic disease can also be risk factors.
Diagnosis
Doctors use a variety of different evaluations to diagnose this condition. These may include:
Medical history and Physical Exam: Your doctor will ask you about your symptoms, medical history, and family history. This can help them identify diagnosed or undiagnosed conditions that might be contributing to your symptoms.
Nerve conduction test and electromyography: Your doctor might recommend a nerve conduction test along with an electromyography. These two tests can be used to rule out large fiber peripheral neuropathies, which can cause similar symptoms. These tests do not evaluate the small nerve fibers and are often found to be normal in people with SFN.
Skin biopsy: Skin biopsies are the most effective way to diagnose small fiber neuropathy and are currently the gold standard for diagnosis. They’re only mildly invasive and can be performed quickly in an outpatient clinic.
During the procedure, the physician will remove 2-3 3mm skin samples, typically from the legs. The samples are then examined under a microscope for signs of small fiber neuropathy.
Our clinic performs the biopsies onsite and sends them to Therapath, a CLIA certified lab for processing.
Reflex testing: Quantitative sudomotor axon reflex testing (QSART) tests autonomic function and is often performed alongside other autonomic function test often referred to collectively as “tilt table testing.” It measures the amount of sweat produced when the skin is stimulated with a mild electrical shock. People who have small fiber neuropathy are more likely to have low sweat output. This along with the other tilt table tests may be used alongside skin punch biopsies in SFN, to quantify autonomic dysfunction. However, they may be found to be normal in individuals with diagnosed SFN and are therefore considered adjunct tests.
Other tests: Your doctor might use other tests to identify or rule out medical conditions related to your symptoms. Blood tests, genetic testing, and imaging tests are other common diagnostic tests.
Treatment
Treatment depends on the underlying condition if any is found. For example, if another medical condition is diagnosed in the evaluation of your SFN, treating that condition will in turn improve the SFN.
However, as noted above in nearly half of the cases, no cause is found and treatment is then focused on symptom management and overall wellbeing.
Pain-related symptoms are typically treated with medication, including:
- Antidepressants: SSRIs, SNRIs and TCAs have all proven to be very beneficial
- Anticonvulsants: These are traditionally considered seizure medications but have been found to be beneficial in nerve pain.
- Corticosteroids: These are often reserved for severe cases for short periods of time given side effects.
- Topical pain creams: Capsaicin in particular can be helpful or topical lidocaine
- Analgesics
Autonomic symptom treatment often depends on what systems are being affected. Often patients respond well to conservative measure such as:
- Graduated Exercise programs. This is imperative as deconditioning can worsen SFN. This program that was designed for POTS is particularly good for anyone with autonomic dysfunction and deconditioning: https://www.dysautonomiainternational.org/pdf/CHOP_Modified_Dallas_POTS_Exercise_Program.pdf
- Adequate and regular hydration: A minimum of half your body weight in ounces of water each day and more if you are in hot climate or exercise.
- Increased salt intake
- Compression stockings with addition of abdominal binder if those alone aren’t sufficient.
- Cognitive behavioral therapy and breathing exercises.
- Low dose propranolol can be beneficial in cases of tachycardia and/or anxiety.
- SSRIs and SNRIs can be helpful though depending on the patient can make some autonomic symptoms worse, therefore medications are initiated at low doses and slowly titrated up.
In severe cases medications such as Fludrocortisone or Midodrine may be used to help with hypotension. These are never used as first line though.
Outlook
Most people with small fiber neuropathy experience a slow progression of symptoms and typically a plateau. In some cases of SFN with time symptoms may resolve completely on their own. Other patients will experience “flares,” of symptoms and have periods of time in which they feel better than others. A diagnosis of small fiber neuropathy doesn’t mean you’ll be diagnosed with large fiber neuropathy later on and does not mean you will have other neurological disorders develop in the future.
Neuropathic pain may worsen over time, though in other cases, it goes away on its own. In general, most people with small fiber neuropathy need to manage some degree of ongoing symptoms.
Small fiber neuropathy can vary widely from mildly bothersome to extremely painful/limiting. This variability can be frustrating for patients and may lead to a sense of loss of control over their bodies. It is important to keep a journal of good days and bad days and to start to notice what makes the symptoms worse or what makes them better. Many people will find that they have flares when they are sick or their bodies are stressed in some other way. Certain food or environmental sensitivities may also contribute. Hormonal fluctuations and seasonal fluctuations may affect symptoms as well. Overall health and wellbeing positively affects all chronic health issues, especially SFN and therefore focusing on exercising, mental health and eating healthy is often the single best thing that can be done.
For a list of Neuropathy support groups visit: https://neuropathycommons.org/content/neuropathy-support-groups